Cataracts
Common Symptoms
- Cloudy or blurry vision
- Colors seem faded
- Glare and halos. Headlights, lamps, or sunlight may appear too bright
- Poor night vision
- Double vision or multiple images in one eye
- (This symptom may clear as the cataract gets larger)
- Frequent prescription changes in your eyeglasses or contact lenses
Surgery Process
Cataract surgery involves removing the natural lens of the eye that has become cloudy and opaque, and implanting an artificial lens, typically made of acrylic. Today, cataract patients have many options and choices! Patients can choose how they want the cataract removed and how they want to see after surgery.
Questions to Ask Yourself
Simply put, the method of removing a cataract has advanced tremendously. Patients are now able to choose between the standard, traditional method of cataract surgery involving handheld blades and instruments or an advanced laser-assisted, bladeless surgery, known as ReLACS.
Traditionally, incisions in the cornea are made using handheld blades to access the cataract. ReLACS (Refractive Laser-Assisted Cataract Surgery) uses femto-second laser technology to precisely create all incisions, a perfectly circular opening in the lens capsule, break-up and soften the hard cataract, and reduce astigmatism. Patients do very well with both procedures, however the accuracy and reproducibility of the femto-second laser allows for a more predictable and precise visual outcome. The traditional approach is a tried-and-true technique that allows patients to do very well after surgery and is covered by insurance companies.
ReLACS allows for a quicker recovery and reduced dependence on glasses; this method however is not covered by insurance companies at this time.
HOW DO YOU WANT TO SEE AFTER SURGERY?
At the time of cataract surgery, an Intra-Ocular Lens (IOL) will be implanted into the eye. The type of lens implant you choose will, in part, determine how you see after surgery. Traditionally, the need for glasses was almost a given after cataract surgery.
Over the last decade, however, technology within cataract surgery has experienced tremendous leaps and bounds; now, we are not only able to correct your cataract, but we are able to correct your vision at the same time. A variety of lens choices allow patients to customize their visual outcome! Choices include a standard monofocal IOL, a Toric IOL, a Multifocal IOL, and an Extended Depth of Focus (EDOF) IOL.
The standard monofocal design is a single-vision lens and thus most patients will need glasses to optimize their vision for near, intermediate, and far distances. The standard monofocal lens is covered by insurance. For patients with astigmatism, the Toric IOL significantly reduces and may even eliminate this type of refractive error; patients who receive this implant may simply need over-the counter reading glasses for near vision and benefit from sharp, clear distance vision.
For patients desiring the least dependence on glasses, the Multifocal and EDOF IOLs are today’s best options when considering cataract surgery. For the right candidate, these lenses give great, “get-around” vision – near, intermediate, and far vision all without the need of spectacles. Occasionally, a cheap pair of “cheaters” may be necessary for very fine print, but most patients are amazed at their newfound independence.
Cataract Lens Guide
As we discussed earlier, once your cataract is removed a new lens implant is inserted into the eye. There are several IOL (intraocular lens) options available. It is important to familiarize yourself with the options you have, so that we can make the best decision
for you and your vision going forward.
MONOFOCAL ASPHERIC
These lenses correct vision for a single distance, either distance or near. The majority of patients with this lens implant will need glasses to see clearly. This lens does not correct for astigmatism (misshaped surface of the eye that causes distorted vision) or presbyopia (loss of near vision that occurs with age). These lenses are the only IOLs covered by medical insurance.
TORIC MONOFOCAL
These lenses correct vision for a single distance, either distance or near, while also correcting for astigmatism. Remember, astigmatism is the misshaped surface of the eye that causes distorted vision. The result is clear, crisp distance vision. Many patients simply need over-the-counter reading glasses for near vision, and some may opt for mono-vision to reduce the need for readers. Mono-vision is the term used when one eye is corrected for distance and the fellow eye is corrected for near; the result is a blended vision which significantly reduces the need for glasses.
EXTENDED RANGE OF VISION IOL
These lenses are meant for patients with an active lifestyle who want great distance and intermediate vision, but who don’t mind wearing glasses for near activities. The lens material allows for a continuous distribution of light from distance and intermediate focal points, and allows for an improved continuity of vision between daytime and nighttime. The design, in turn, has a low incidence of halos and glare. This lens corrects for presbyopia and astigmatism, if needed. As above, this lens may not be appropriate in patients who have had vision correction in the past, such as LASIK, PRK, and RK.
MULTIFOCAL IOL
These types of lenses are designed to be able to provide patients the ability to see objects clearly at different distances without glasses—near, far, and in between. The lens material distributes light to different distances, which the eye can focus on for sharper vision. For people who are active and find wearing glasses inconvenient, this lens may be the optimal choice. This lens corrects presbyopia, and may also correct for astigmatism, if needed. A con of this lens design is potential nighttime glare and halos. This lens type may not be appropriate in patients who have had vision correction in the past, such as LASIK, PRK, or RK.
LIGHT ADJUSTABLE LENS (LAL)
This lens is the first and only lens that can be customized after cataract surgery. The LAL is an adjustable, rather than fixed, lens whereby you have the ability to adjust the lens prescription and vision to your unique preferences and lifestyle requirements. The intraocular lens (IOL) is made of a special photosensitive material that changes the shape and power of your implanted lens in response to ultraviolet (UV) light to optimize your vision. A Light Delivery Device (LDD) non-invasively delivers UV light to precisely reshape the lens based on the visual correction that is needed to target your custom prescription. UV light treatments will be performed in your our office after your eye has healed.
Depending on your desired visual outcome, you may have 1–3 light treatments, followed by two “lock-in” treatments to prevent further changes. The fine-tuning process may take several weeks during which you will have to wear UV protective glasses. The LAL may be adjusted for distance, intermediate, and near and has a low incidence of glares and halos. This is an excellent option for those who have had previous refractive surgery, such as LASIK, PRK, or RK!
Special Considerations
DO YOU HAVE A HISTORY OF VISION CORRECTION SURGERY (LASIK, PRK, RK)?
Patients with a history of vision correction surgery (LASIK, PRK, RK) do very well with cataract surgery, however there are a few considerations to keep in mind. Vision correction surgery changes the shape and contour of the cornea to allow patients to see well at the time of surgery. At the time of cataract surgery, however, the prior surgery reduces the accuracy and predictability of not only the pre-operative measurements, but also the surgical outcomes. Additionally, patients with a history of vision correction ARE NOT good candidates for advanced lens implants, such as the Multifocal or Extended Depth of Focus IOLs; implanting these types of lenses will result in increased glares and haloes, and may reduce the quality of vision. The BEST option for those with previous refractive surgery looking for independence with glasses is the Light Adjustable Lens (LAL).
HOW DO WE OVERCOME THESE ISSUES IN PATIENTS WITH A HISTORY OF VISION CORRECTION?
There are three primary procedures our office implements to give patients with a history of vision correction the highest chance of visual success:
- Pre-operative discussion: In our experience, the most important part of the surgical process in patients who have a history of vision correction surgery is a lengthy and detailed pre-operative discussion. It is important to understand that the measurements taken prior to surgery may not be as accurate and predictable; these patients may still need some level of spectacle correction after surgery. Identifying obstacles prior to surgery puts patients more at ease and they are much more comfortable throughout the process as they will know what to expect.
- ORA (Optiwave Refractive Analysis): This is a device that allows on-demand power calculation and is used to ensure proper implant power, IOL placement, and/or determination of the magnitude and direction of astigmatism. The device takes 40 real-time measurements to validate the correct targeted IOL (intraocular lens). The measurements are taken after your cloudy cataract is removed and prior to implantation of the lens. This device may be used during any type of cataract surgery, but is most helpful in patients who have a history of vision correction surgery. In order to achieve the highest level of success, all patients who have a history of vision correction will undergo this measurement at the time of cataract surgery. Since this is a custom option, the use of this device is not covered by your insurance, and the additional out-of-pocket fee is $250.
- Post-cataract surgery enhancement: Despite a thorough pre-operative discussion and use of ORA technology, some patients still fail to reach the target correction after surgery. In these patients, the initial management is observation for up to 3-6 months; oftentimes, the target will drift back to the expected correction. If this does not occur, Dr. Patel can perform an enhancement using PRK (photorefractive keratectomy) to correct the residual refraction. This procedure is similar to your vision correction surgery you had many years ago and allows patients to achieve the target visual outcome. If a patient does not want an additional enhancement, many patients can be corrected with a pair of prescription glasses. It is important to know that enhancements are rarely needed. If required, the enhancement is a separate, non-covered, procedure and the out-of-pocket fee is $1200.
- Light Adjustable Lens: Implantation of the LAL overcomes all of the prior considerations, as this Intraocular Lens is fully customizable after cataract surgery. This is considered the gold-standard option for post-refractive patients. The intraocular lens (IOL) is made of a special photosensitive material that changes the shape and power of your implanted lens in response to ultraviolet (UV) light to optimize your vision. A Light Delivery Device (LDD) non-invasively delivers UV light to precisely reshape the lens based on the visual correction that is needed to target your custom prescription. UV light treatments will be performed in your our office after your eye has healed. Depending on your desired visual outcome, you may have 1–3 light treatments, followed by two “lock-in” treatments to prevent further changes. The fine-tuning process may take several weeks during which you will have to wear UV protective glasses.
HOW DOES DRY EYE SYNDROME AFFECT CATARACT SURGERY?
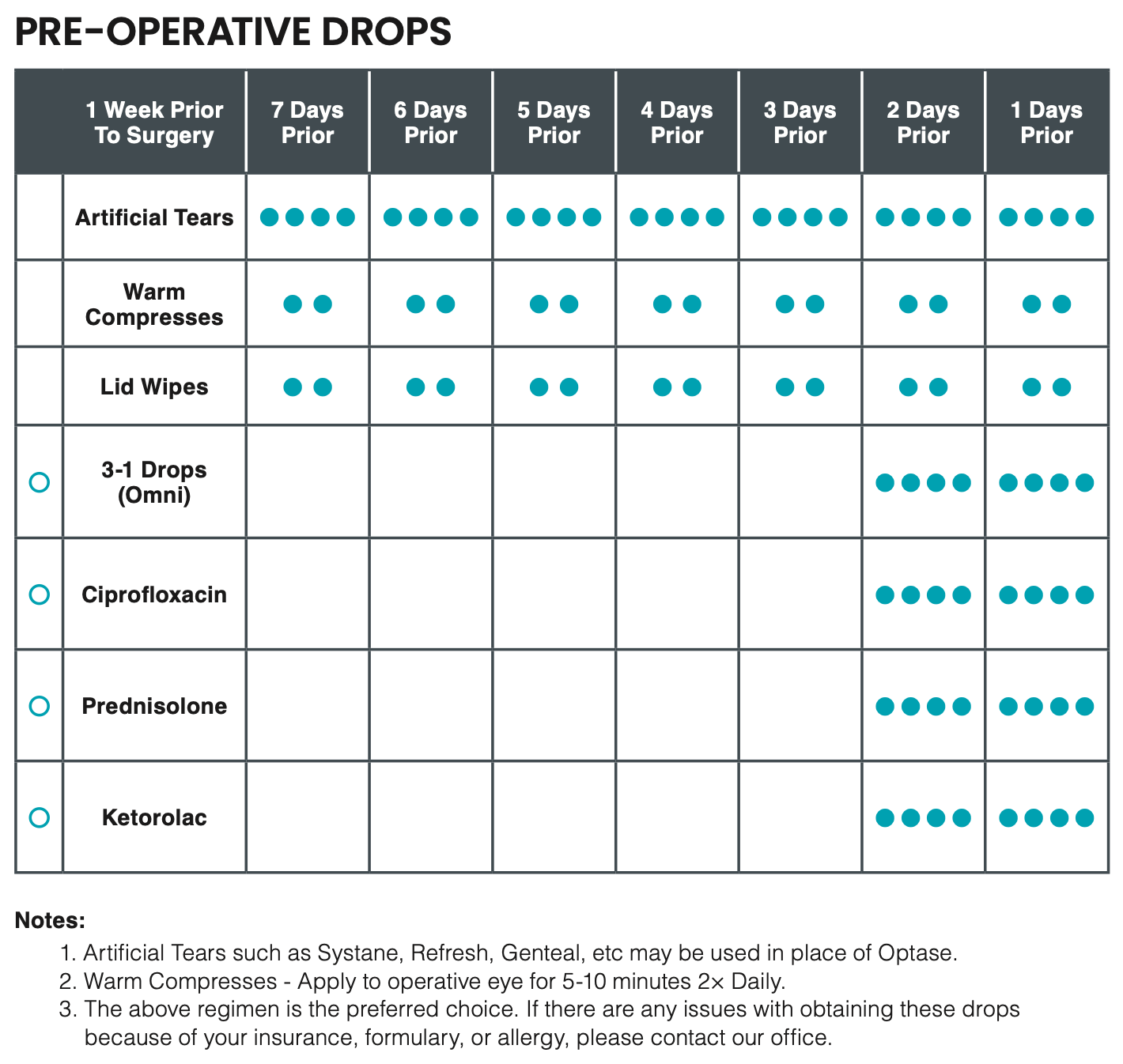
Dry Eye Syndrome is a very common condition that affects the ocular surface as a result of not having enough tears to lubricate the eyes or simply having poor quality tears. During every cataract evaluation, we look for signs and symptoms of dry eye. Treating dry eye before cataract surgery will stabilize the ocular surface and increase the accuracy of the preoperative IOL measurements. If the dry eye is severe, punctal plugs or a prescription drop (Xiidra or Restasis) can be used a few weeks before surgery to improve the ocular surface.
While there may not be an actual cure for dry eye, preparing your ocular surface prior to anticipated cataract surgery will certainly minimize post-operative complaints and maximize results. For patients with moderate-to-severe dry eye disease, pre-operative treatments with heat-based and/or laser-based modalities may significantly improve the accuracy of the pre-operative measurements and enhance visual outcomes and recovery.
The TearCare® System is intended to treat the ocular surface of patients with evaporative dry eye disease due to meibomian gland dysfunction (MGD). The treatment applies localized heat therapy to the meibomian glands, followed by manual expression of the glands. The treatment is an in-office procedure, and lasts 15-20 minutes. The cost is $600 per treatment, and is a non-covered procedure.
BroadBand Light (BBL™) is a high-quality, enhanced IPL modality that uses polychromatic, non-coherent, continuous light waves from the visible (420 nm) to the infrared (1400 nm) spectrum to treat poor tear film quality and meibomian gland inflammation. The treatment is an in-office treatment, and lasts 30 minutes. The cost is $400 for a single treatment, or $900 for three monthly sessions (may be recommended for those with severe ocular surface disease).
The procedure is not covered by insurance at this time.
WHAT IS MONOVISION (BLENDED VISION)?
Most people have a dominant eye (one that you prefer to see with if you had to close one eye). With monovision, the vision in your dominant eye is corrected for distance vision, while your other eye is intentionally left somewhat nearsighted to allow you to see close objects. Both eyes still work together, allowing you to see clearly at any distance. While this way of seeing may sound complicated, many people find they adapt well to this technique. In fact, with both eyes open, they may not be able to tell which eye is set for distance and which is set for near.
However, monovision is not for everyone. Some people find they simply cannot adapt to it. This is why Dr. Patel usually recommends trying monovision with contact lenses first before committing to surgery for presbyopia with monovision IOLs as part of cataract surgery.
If you are considering monovision—or blended vision—keep in mind that because one eye is focusing at one distance while the other is focused at another, you may lose some depth perception. Also, you might still need to use reading glasses in certain cases, such as reading small print.
Cataract Surgery Choices
CUSTOM PACKAGE
Test drive your newest vision, and fine-tune it to YOUR specifications! This package incorporates light adjustable technology and extended depth of field optics. Using the LAL technology, we have the ability to adjust the lens prescription and vision to your unique preferences and lifestyle requirements after surgery. Depending on your desired visual outcome, you may have 1–3 non-invasive light treatments, followed by two “lock-in” treatments to prevent further changes. The fine-tuning process may take several weeks during which you will have to wear UV protective glasses. This option provides the most custom quality and range of vision! Test drive your vision and live your best life on your terms!
Vision: Distance, Intermediate, Near
LIFESTYLE PACKAGE
Live life to the fullest (and make sure you have the vision to go along with it!)! This package incorporates the best technology in multi focal and extended depth of field optics, along with femto-second laser technology to provide the best quality and range of vision! Whether you love playing golf, reading, knitting, traveling or playing with your grandkids, you can enjoy the majority of your day without the hassle of glasses!
Vision: Distance, Intermediate, Near
ACTIVE PACKAGE
Don’t mind wearing readers, but want the best quality distance vision to see your golf ball or watch your favorite movie? This package incorporates the best quality monofocal+ lens and significantly reduces or eliminates astigmatism, while using femto-second laser technology to provide the best long-distance vision!
Vision: Distance, Intermediate
TECHNOLOGY PACKAGE
Femto-second laser technology has become the most precise and accurate method to remove cataracts and provide outstanding and reliable outcomes! This package incorporates the latest in laser technology to assist in cataract removal, and implantation of a standard monofocal lens. Patients will experience the highest levels of laser technology and safety, while having a reduced dependence on glasses.
Vision: Distance
STANDARD PACKAGE
You love how glasses look on you, and you’re the first to choose a new set of frames that complement your beautiful smile! Traditional manual cataract surgery has been the norm for many years. This package incorporates basic cataract surgery and implantation of a standard monofocal lens. Although manual surgery with blades is not as accurate as a laser, Dr. Patel has optimized his results using micro-incisions to ensure the best outcomes. Patients can expect to wear glasses full-time.
Vision: None (Patients will need prescription glasses)
INSURANCE COVERAGE
Cataract surgery costs are generally covered by Medicare (if you are Medicare eligible) as well as by most private insurance plans. Your cataract surgery costs will be covered by your health insurance as long as your vision tests at a certain level of acuity or clarity.
If you have a private insurance plan, they too may have similar vision requirements that you must meet in order to have your surgery covered.
Even if Medicare or private insurance covers your cataract surgery, there may be some costs you would still be responsible for, such as a package upgrade of your choosing or having cataract surgery before your vision has deteriorated enough to be eligible for Medicare or insurance coverage.
OUT-OF-POCKET COSTS
It is important that you know the full spectrum of your potential costs. Your out-of-pocket costs may include copays, co-insurance, surgery center co-pays, anesthesia fees, as well as any upgrades you may choose.
The total amount can vary depending on the details of your particular plan.
You should contact your plan for the most accurate estimates. Our office will always be available to assist you in this process.
Appointment Expectations
PRE-OPERATIVE MEASUREMENTS AND COUNSELING
During this visit, sophisticated corneal and intra-ocular lens measurements and power calculations will be performed. Contact lens wear may cause an error in the results of the implant power measurement. Because of this, soft contact lenses must be removed one week prior to appointment and hard contact lenses must be removed two weeks prior to appointment.
You, our refractive surgery counselor, and Dr. Patel will formulate a plan to give you the vision you want! At this visit, we will discuss insurance benefits, out-of-pocket costs, surgery scheduling, and pre- and post- operative instructions! Come prepared with questions!
PRE-OPERATIVE CLEARANCE
Physical examination and EKG with your Primary Care Physician (PCP) and/or Cardiologist (if you have any history of heart conditions). Schedule this appointment as soon as possible with your primary physician and/or cardiologist. Your pre-surgical clearance needs to be completed within thirty days of surgery.
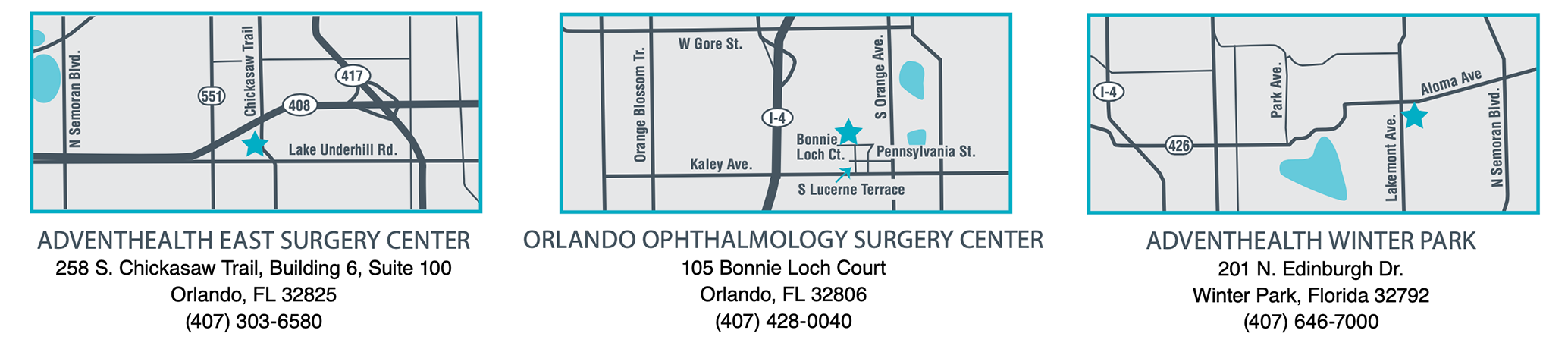
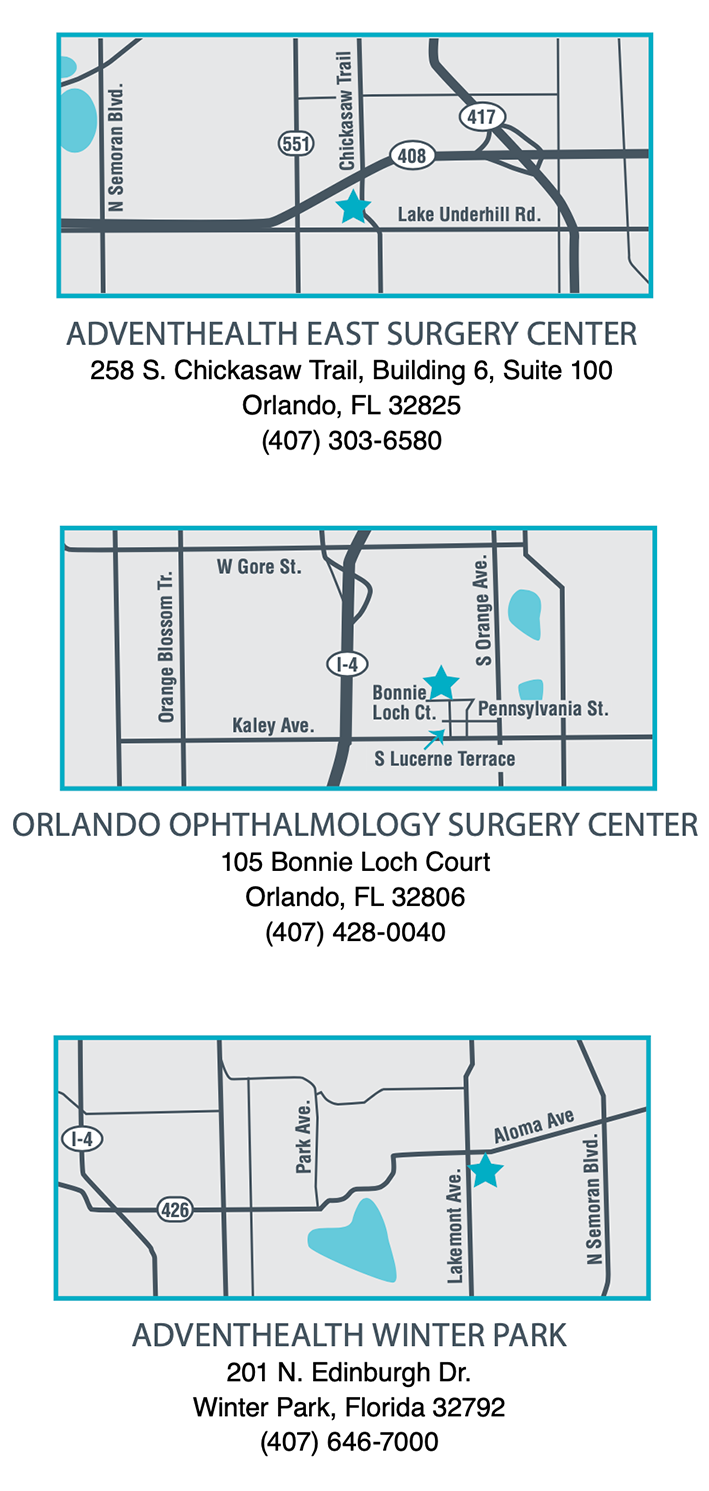
SURGERY
Your surgery will be performed at one of our surgery centers: AdventHealth East Surgery Center or Orlando Ophthalmology Surgery Center (OOSC). The date and time of your surgery will be scheduled at our office. Prompt arrival to the appropriate center will ensure a smooth day of surgery.
POST-OPERATIVE APPOINTMENTS
All post-operative appointments will be at our office. You will be seen a day, a week, and a month after your surgery. These appointments are very important to ensure that the healing process is progressing appropriately.
TRANSPORTATION
Arrange transportation to and from the surgery center for the day of surgery and the day after surgery. Due to anesthesia and state laws, you must have someone to accompany you and are unable to use ride- sharing, such as Uber, Lyft, etc. Please be flexible, it may be necessary to adjust your arrival times.
Pre-op Instructions
- Do not eat or drink anything (including coffee) 8 hours prior to surgery.
- Any oral medicines that you normally take in the morning may be taken with a very small sip of water, on the morning of your surgery. All diabetics should contact their PCP on how to manage their insulin on the day of surgery.
- Do not wear makeup the day of your surgery.
- Report to the hospital two hours prior to your scheduled surgery time. The hospital will tell you the exact time to arrive when they call to remind you before surgery.
- You must have a driver to drive you home after surgery.
- Keep tip of eye dropper clean and do not touch tip to the eye or any other object.
- Wait five minutes between each different eye medication.
- Each medication has refills if needed.
Post-op Instructions
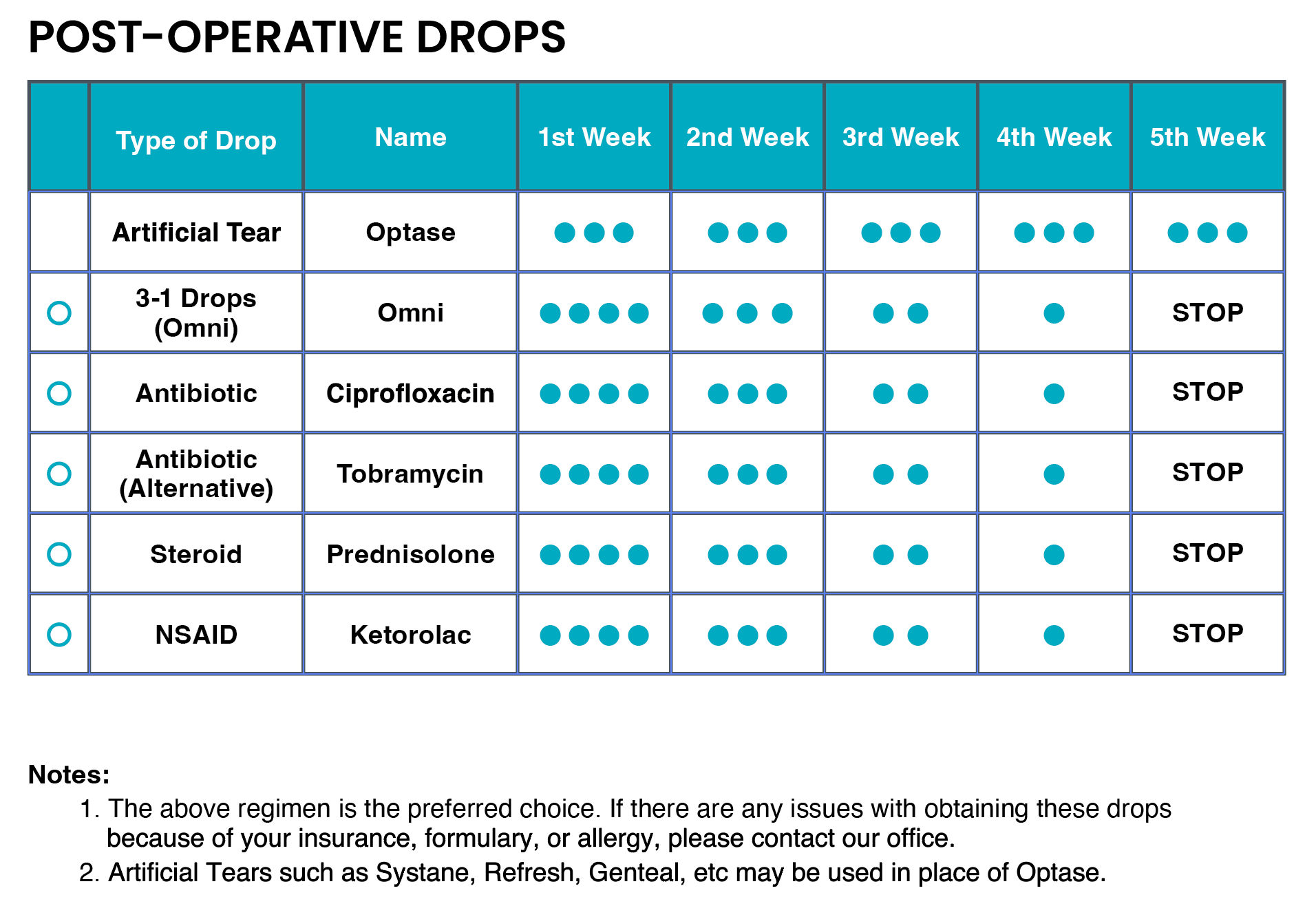
- Day one of your eye medications starts immediately after you arrive home from surgery.
- Wear shield at night for one week.
- Use warm water or warm soapy water to cleanse around eye.
- Do not rub eye for one week.
- Keep eye closed while showering for one week.
- Do not get water in the eye for one week.
- No make-up around eye for one week.
- You may NOT bend at the waist or perform strenuous activity for approximately 1 week after the surgery.
- You have no restrictions after one week.
- You may drive when you feel your vision is adequate.
- No vigorous exercise (including swimming) for one week.
- You may return to work five days after surgery. Ask doctor if you wish to return sooner.
- Keep tip of dropper clean and do not touch tip to eye or any other object.
- You may experience a foreign body sensation in the eye for several weeks after surgery.
- It takes approximately one month to get your best vision. Your vision will be blurred while your eye is healing.
- Your eye may be dilated for 2-3 days after surgery.
Surgery Centers
The eye functions just like a camera – it has a natural lens inside the eye to help focus light clearly onto the retina (like the film of a camera). A cataract is the clouding of the natural lens in the eye; so when something is disrupting the lens, it is hard to get a clear picture.
The cataract is a result of a buildup of proteins in the natural lens. Just as a smudge on the lens of your camera prevents light from focusing clearly and producing a clear image, a cataract does the same.
Everyone will develop a cataract some point in their lives. Certain risk factors can accelerate the progression of a cataract such as smoking, diabetes, and steroids.
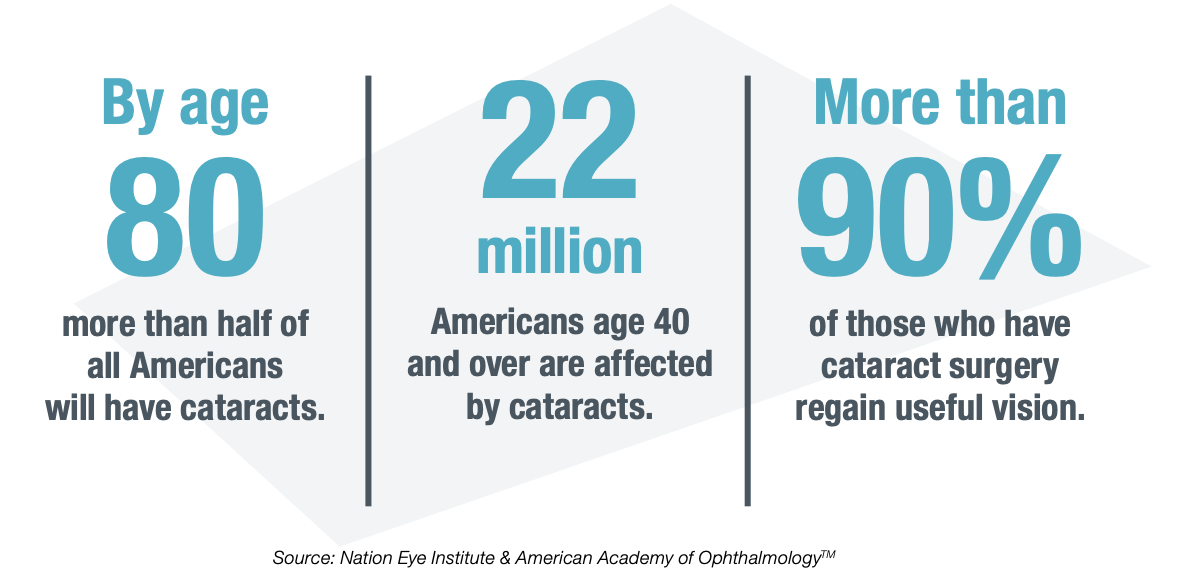
Cataract Fast Facts:
- Cataracts affect nearly 22 million Americans age 40 and over
- By age 80, more than half of all Americans will have cataracts, according to the National Eye Institute
- More than 90 percent of those who have cataract regain useful vision
- Cataracts are formed when some of the protein that makes up the lens clumps together and clouds a small area of the lens
- Cataracts are not preventable, but they are treatable
- Most commonly related to aging

Cataract Prevention
Although there is no known way to prevent cataracts, there are ways to slow the process of cataract development. These include:
- Not smoking
- Wearing a hat or sunglasses when you are in the sun
- Avoiding sunlamps and tanning booths
- Eating healthy foods
- Keeping diabetes under control
Cataract Treatment Options
Early cataracts may be treated with a simple change in your eyeglass prescription, however as the cataracts progress a new eyeglass prescription may no longer be effective in minimizing the effects of the cataracts on your vision.
For visually significant cataracts that are no longer correctable with eyeglasses, the mainstay of treatment is Cataract Surgery.
No-Stitch, Small Incision Cataract Surgery
This is, by far, the most common method for cataract surgery. During the procedure, your Ophthalmologist will remove the natural lens in your eye that has become cloudy (cataract) by way of small incisions and ultrasound. Your surgeon will then implant an artificial lens (IOL, or intraocular lens) to focus light onto the retina just like the previously removed natural lens did.
Lens Options
Over the last five years, cataract surgery has achieved remarkable new standards. Ophthalmologists are not only able to correct the cataract, but now are also able to correct one’s vision (such as Astigmatism, or Glasses). Lens options discussed prior to surgery will allow the patient to determine what he or she would like to achieve. The main purpose of these lenses is to achieve spectacle independence and provide a great range of vision without the need for glasses. These advanced technology lenses are able to offer patients convenience, comfort, and safety.
After Surgery
With the surgery, most patients will undergo a healing process. With the administration of eye drops, most patients will see better each day after surgery with clear, unobstructed vision appearing by day 7-14. Depending on your lens selection, you may not even require prescription eyeglasses! After the surgery, most patients are able to resume his or her normal activities within days.
Surgery Centers
We participate with three surgery centers to give each patient a variety of options from location, time of surgery, and insurance coverage. Below you will find the name, address, and contact information for each of our surgery centers. Be sure to confirm which center your surgery will be performed at.
What People Are Saying
Kee Nikol2024-01-22I had a really great experience. The office is beautiful and very clean. The staff were all very kind and professional. Dr. Ahmed was very friendly, funny, and made me feel immediately comfortable. He did a fantastic job explaining things to me in a way I could understand. I highly recommend him!Pradeep Raval2024-01-22Very caring and professional team of eye specialists.M Ax2024-01-19Lake Nona ophthalmology is excellent! Had both eyes cataract surgery with Dr. Payel and I highly recommend.Susie2024-01-18I am elated with the care my mother received from Dr. Ahmed and staff today. We needed additional assistance transferring my mother from her wheelchair to and from the examination chair. Both the doctor and another staff member transferred her. The treatment Dr. Ahmed prescribed is conservative and more agreeable than her previous ophthalmologist’s recommendations. The office staff is top-notch, too. They were exceedingly kind, gracious and generous with us at every turn, especially after a stressful afternoon. I am relieved to feel positively about my mom’s optical care going forward. Thank you, Dr. Ahmed and staff, for the best-in-class care!Julianne VanLaningham2024-01-18Dr.Patel is a competent ophthalmologist. He is also a kind person who takes time with his patients and listens. I highly recommend him as an ophthalmologist!Tina Droege2024-01-17The staff are very friendly, and the Dr Patel takes his time and always ask how are you been feeling!Carmen Rosado2024-01-12Excellent service and very nice staff!
GET STARTED TODAY
At Lake Nona Ophthalmology, Dr. Patel and his team provide compassionate, excellent care and treatment for patients throughout Central Florida.